Produced on behalf of the British Association of Sport and Exercise Sciences by Profs Greg Whyte OBE, FBASES and Mike Tipton MBE, FTPS.
Background and evidence
Environmental conditions can have a profound impact on human performance and health. Excessive cooling can impair performance and cold is one of the largest killers of sports people in the UK (Whyte et al., 2014). Accordingly, management of the cold is important. This expert statement examines the impact of cold environments on performance and health, and ways of mitigatingthese problems.
Performance
Performance in the cold can be impaired by cooling of nerves, muscles and deep body temperature. Below a local tissue temperature of 20˚C the firing rate, conduction velocity, amplitude and repolarisation of action potentials is slowed. Nerve block can occur at local temperature of 5-15˚C for 1-15 minutes and maximum power output falls by 3% per ˚C fall in muscle temperature, with physical incapacitation occurring at a temperature of about 27˚C (Castellani & Tipton, 2015). The rate of force application is particularly affected with an increased motor unit recruitment to maintain force production (left shift in EMG power frequency). Muscle spindle activity, twitch force and stretch reflexes are decreased. Enzymatic activity, rate of ATP utilisation, acetylcholine and calcium release and uptake, and muscle tendon elasticity are all reduced. Reductions in muscle blood flow result in an earlier contribution from anaerobic metabolism, higher plasma lactate concentrations and a shorter time to exhaustion (Whyte et al., 2014).
With a reduced deep body temperature, the superimposition of shivering on low intensity exercise metabolism increases the oxygen consumption and cardiac output for any given submaximal workload; thereby decreasing exercise economy, increasing carbohydrate oxidation rates and hastening glycogen depletion and fatigue (Castellani & Tipton, 2015). A decrease in deep body temperature of 0.5˚C-1.5˚C results in a reduction of 10-40% in the capacity to supply oxygen to working muscles due, in part, to a left-shift in the O2 dissociation curve. With more profound muscle cooling, anaerobic energy production is impaired. Maximum oxygen consumption (V˙O2max) is reduced by 10-30% following a 0.5-2˚C fall in deep body temperature. Stride frequency increases and stride length decreases, concomitant with an increase in slips, trips and falls (Whyte et al., 2014).
Dehydration is common in cold environments because thirst is blunted, water is not always easily available (frozen) and respiratory water loss can be high in cold dry environments. Cold exposure can also result in a cold-induced diuresis due to vasoconstriction and raised central venous pressure; although this can be prevented by moderate intensity exercise (Whyte et al., 2014). In addition to a performance decrement, the combination of exhaustion (cessation of exercise), hypoglycaemia, dehydration and hypothermia can represent a significant health threat during exposure to the cold (Golden & Tipton, 2002).
Health
Threats to health in cold air environments include: frostbite, non-freezing cold injury and hypothermia. Additional threats in cold water resulting from its greater cooling capacity include: cold shock leading to drowning and cardiac issues (Whyte et al., 2014). A number of pre-existing conditions (e.g. asthma, Raynaud’s disease, hypertension) can be exacerbated by exposure to cold environments. Prolonged working in the cold can result in hypertension, mild respiratory impairment (airflow limitations, bronchial hyper-responsiveness) and increased incidence of musculo-skeletal complaints (Tipton, 2019).
Frostbite and non-freezing cold injury
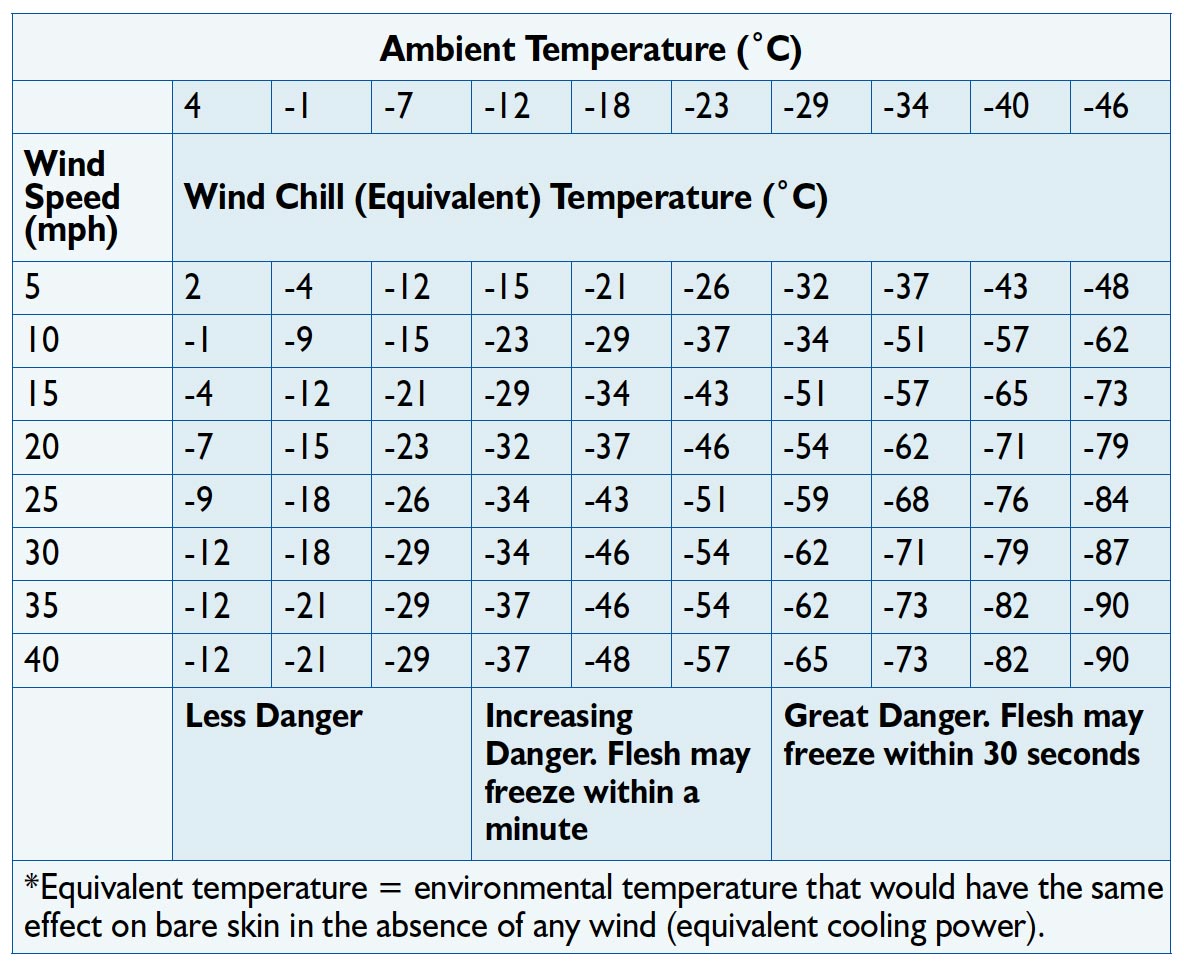
Skin cooling is accentuated by peripheral vasoconstriction. The extremities that are most affected due to their high surface area to mass ratio, and the fact that their major source of heat, blood flow, has been restricted. The incidence of cold injury begins to increase when air temperatures fall below -12˚C and wind speed exceeds 4.5 m.s-1 (see Table 1). These thresholds are reduced at altitude due to augmented vasoconstriction caused by hypoxia. Females and individuals of African descent are more at risk of cold injury due to differences in the thermal sensitivity of their peripheral circulation (Whyte et al., 2014).
Frostbite. Human tissue freezes at -0.53˚C. With rapid cooling, intracellular freezing occurs and ice crystals cause direct mechanical disruption of the tissues. Slow cooling causes predominantly extracellular water crystallisation. Osmotic outflow then leads to intracellular dehydration, damage to capillary walls and cell death. Local hypoxia and the release of inflammatory mediators result in increased blood viscosity, capillary sludging, endothelial injury, platelet aggregation, vessel thrombosis and gangrene (Francis & Oakley, 1996).
Non-freezing cold injury. The pathogenesis and pathology of non-freezing cold injury is less understood. Prolonged exposure to cold and cold/wet condition can result in life-long cold sensitivity, hyperhidrosis, intractable pain, bone/joint damage and gait changes. These symptoms probably result from small fibre neuropathy (due to direct cooling) and local vascular endothelium damage (due to cold-induced ischemia) (Whyte et al., 2014).
Hypothermia
Defined as a fall in deep body temperature below 35˚C, the clinical features of hypothermia include:
• Mild (35-32˚C) – shivering, mild incoordination, cold axilla, tachycardia, tachypnea, diuresis, amnesia.
• Moderate (31-28˚C) – apathy, clumsiness, slurred speech, weakness, semi-consciousness, fatigue, dehydration.
• Severe (<28˚C) – bradycardia, cardiac arrhythmia, ventricular fibrillation, hypotension, pulmonary oedema, muscle rigidity, fixed dilated pupils, and possible fatality (Francis & Oakley, 1996).
There are many risk factors for hypothermia, including: climatic conditions, age, body stature/morphology, sex, fitness, nutritional status, fatigue, injury, intoxication and clothing (Whyte et al., 2014).
Water immersion
On initial immersion rapid cooling of the skin initiates “cold shock” that includes: a “gasp” response, hyperventilation, hypertension and increased cardiac workload. These can be precursors to drowning and cardiovascular problems. In situations where the face is also immersed, co-activation of sympathetic and parasympathetic inputs to the heart can produce “autonomic conflict,” resulting in potentially fatal arrhythmias in a variety of sporting situations (i.e. open water swimming, triathlon). Approximately 60% of cold water immersion deaths generally occur within the first minutes of immersion, long before hypothermia occurs (Tipton, 2013).
Mitigating the threats of cold environments
Limiting exposure. Indices (e.g. Table 1 – wind chill) help identify the risk of cold injury. Limiting exposure time and appropriate clothing, hydration, nutrition strategies can reduce the deleterious impact of the cold. International governing bodies of sport have set temperature limits for competition to reduce the risk of injury. Clothing. In air, the heat produced by exercise is usually sufficient to offset that lost to a cold environment, particularly when combined with the careful use of clothing.
Clothing should:
• Prevent flushing of cold air/water beneath the garment
• Trap air close to the skin
• Enable adjustments in insulation (e.g. layers) to cater for changes in heat production
• Be windproof
• Wick moisture away from the body
• Be vapour permeable.
Table 1. Wind chill (effect of wind speed on cooling)
Adaptation and acclimatisation to cold
In water, the cold shock response subsides after 1-2 minutes. It is best to do as little as possible during this period (“float first”) to avoid aspirating the small volume of water necessary (1.5 L salt water) to start the drowning process (Golden & Tipton, 2002).
The most frequently reported acclimatisation is characterised by a reduced shivering response (habituation), faster fall in deep body temperature (“hypothermic adaptation”) and increased thermal comfort. The acclimation is specific to the deep body temperatures experienced during acclimatisation. The hazardous initial responses to cold water immersion can be reduced by as much as 50% by as few as five 2-minute immersions in cold water. This habituation appears to last for several months (Tipton, 2013).
Out of hospital treatment
Mild hypothermia: warm drink, external active re-warming.
Moderate and severe hypothermia: critically ill, handle carefully, passive slow (0.75-1˚C.h-1) rewarming – insulate and evacuate.
Frostbite: evacuate, rewarm only if re-exposure and further trauma are unlikely and follow-up treatment available. Do not rub injured area. Immerse in whirlpool bath with antiseptic added (38˚C) until red/purple colour and tissue is pliable.
Non-freezing cold injury: remove outer clothing (i.e. boots and socks), slightly elevate limb. Insulate area (do not rewarm rapidly), expose to warm air. Encourage movement of affected tissue (i.e. toes and ankles).
Drowning: basic life support compressions and ventilations (2 rescue breaths then cardiopulmonary resuscitation at 30:2 ratio).
Provide high inspired oxygen as soon as possible.
Summary
Cold can decrease performance and threaten health. Limiting exposure, appropriate clothing/protective equipment, hydration and nutrition, and acclimatisation can help mitigate these problems.
Prof Greg Whyte OBE, FBASES
Greg is a Professor of Applied Sport and Exercise Sciences at the Research Institute for Sport and Exercise Sciences, Liverpool John Moores University.
Prof Mike Tipton MBE, FTPS
Mike is Professor of Human & Applied Physiology at the Extreme Environments Laboratory, School of Sport, Health & Exercise Science, University of Portsmouth.
References:
Castellani, J.W. & Tipton, M.J. (2015). Cold stress effects on exposure
tolerance and exercise performance. Comprehensive Physiology, American
Physiological Society Section 14. Handbook of Physiology, Environmental Physiology.
Francis, T.J.R. & Oakley, E.H.N. (1996). Cold injury. In J.E. Tooke & G.D.O.
Lowe (Eds.), A Textbook of Vascular Medicine (pp. 353-370). London: Arnold.
Golden, F. & Tipton, M.J. (2002). Essentials of sea survival. Champaign, Illinois:
Human Kinetics.
Saycell, J. et al. (2018). Scientific rationale for changing lower water temperature
limits for triathlon racing to 12 C with wetsuits and 16 C without. British Journal
of Sports Medicine. 0, 1-8. doi:10.1136/bjsports-2017-098914
Tipton, M.J. (2013). Sudden cardiac death during open water swimming. British
Journal of Sports Medicine, 10.1136/bjsports-2012-092021
Tipton, M.J. (2019). Cold. In P. Brukner & K. Khan (Eds.), Brukner & Khan’s
clinical sports medicine (5th edition), Volume 2 (Exercise Medicine). AU: McGraw-
Hill Education.
Whyte, G., Loosemore, M. & Williams, C. (2014). ABC of Sports & Exercise
Medicine (4th edition). London: BMJ Books.
First published in The Sport and Exercise Scientist, Issue 66, Winter 2020.
Published by the British Association of Sport and Exercise Sciences – www.bases.org.uk




Add comment