Produced on behalf of the British Association of Sport and Exercise Sciences by Dr Jo Corbett, Dr Oliver Gibson, Dr Neil Maxwell, Dr Caroline Sunderland and Prof Neil Walsh.
Introduction
This expert statement presents practical, evidence-based strategies, for able-bodied individuals performing continuous or intermittent exercise (>~30 minutes) in hot environments, defined as environments where exercise is negatively impacted by high thermal-stress.
Background and evidence
Many individuals must exercise in the heat and numerous sporting events take place in hot environments, e.g. the 2020 Olympic Games (Tokyo) and the 2022 World Cup (Qatar). The detrimental influence of heat on prolonged exercise is well established, although the effect is a continuum and depends on the balance between heat-gain and heat-loss; in some circumstances (e.g. high work-rates, humidity, thermal radiation, low airflow) performance is impaired within modest ambient temperatures (≥~15 C).
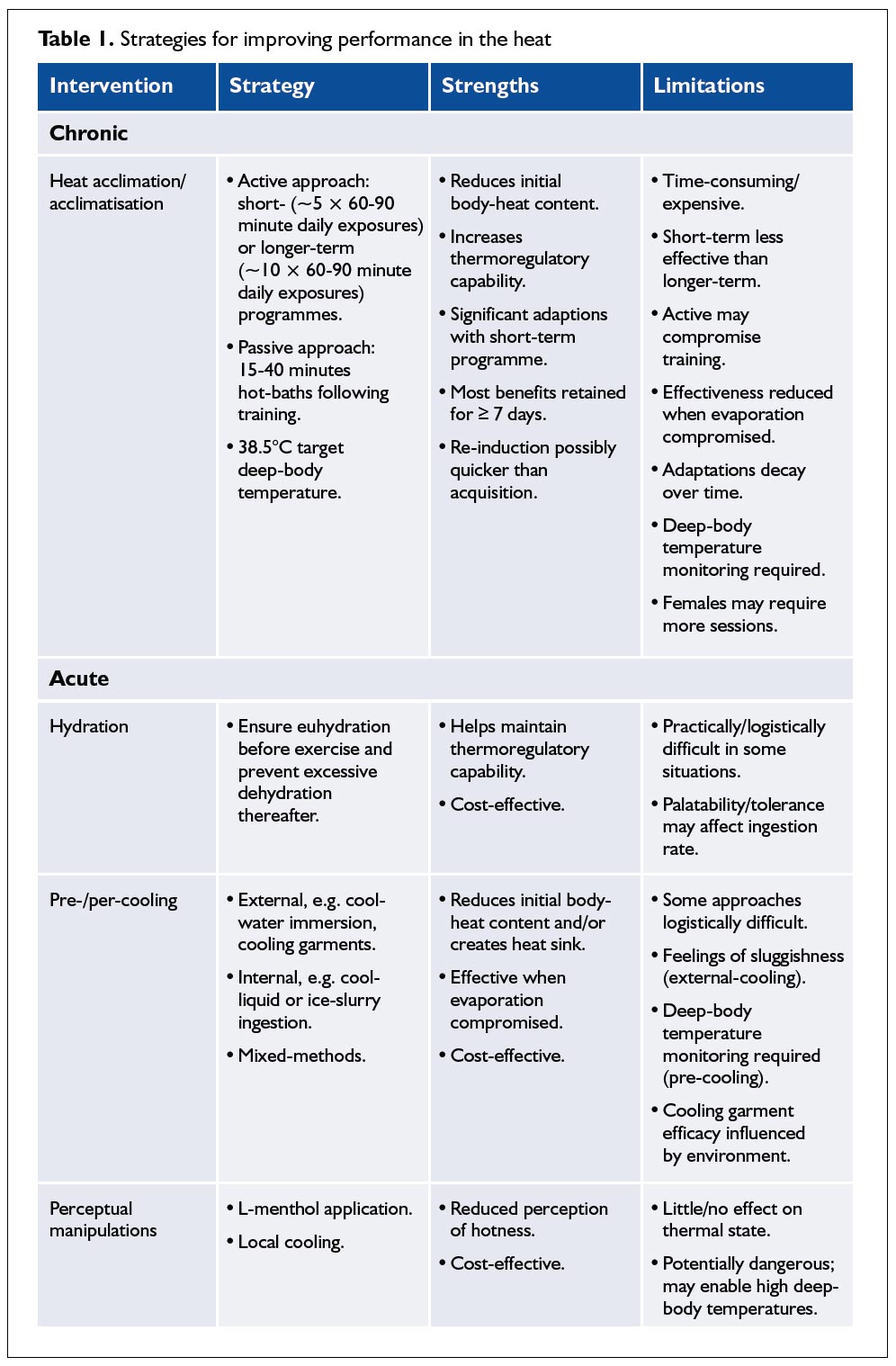
Effective interventions can be administered in the days before (chronic), or on the day of and during (acute) heat exposure and will achieve one, or more, of the following: 1) increased or maintained heat dissipation; 2) reduced initial body-heat content; and 3) altered thermal perception.
Chronic interventions
Heat acclimation/acclimatisation
Acclimation (laboratory) or acclimatisation (natural environment) to heat (HA) reduces initial deep-body temperature and increases heat dissipation rates. This reduces the thermal-strain for a
given external work-rate during exercise in a thermally-stressful environment. HA is a powerful tool for mitigating the effects of heat, although efficacy is reduced in environments limiting sweat
evaporation, such as the microclimates within some protective clothing. Most studies have examined ‘slow’ adaptation (10- 12 days exposure) of men, of modest fitness, in heat-stressed occupations and are less relevant to elite athletes, who are often partly acclimatised and have limited time to devote to HA.
HA is achieved by repeatedly elevating deep-body and skin temperature to a high level that elicits pronounced sweating. This is often achieved through exercise (active approach), either in a hot and/or humid environment or in clothing restricting heat loss, although very humid environments can lead to hidromeiosis (a reduction in sweating caused by blocking of the sweat glands). Passive approaches to HA, e.g. hot-baths (≤ 40 C) of 15 to 40 minutes following training, can be effective (Zurawlew et al., 2016), but as yet unconfirmed as equal to the traditional active HA programmes. The duration and frequency of heat exposures that maximises HA is unknown, although 60-90 minute daily exposures are common when using the active approach. Longer (~10 daily exposures) rather than shorter (~5 daily exposures) programmes are more effective. Nevertheless, shorter programmes result in some significant adaptations and are time efficient (Neal et al., 2016). However, adaptation may be slower in females, who may require longer to achieve the same benefits (Mee et al., 2015).
Maintaining thermal-strain (isothermal-strain) as the individual adapts, through progressively increasing work-rate or environmental stress, should be superior to exercising at a fixed work-rate and environmental stress, where the stimulus for HA diminishes as the individual adapts, although empirical support is lacking (Gibson et al., 2015). Isothermal-strain typically uses higher initial work-rates than fixed work-rate protocols. In thermally-stressful environments this facilitates rapid elevation of deep-body temperature, but thereafter requires little exercise for maintenance, potentially reducing total work; this may be preferable for athletes approaching competition. With all HA approaches deep-body temperature (rectal/oesophageal) should be monitored for efficacy and safety and individuals should be monitored for signs and symptoms of heat-illness. A target deepbody temperature of ~38.5 C is common (Gibson et al., 2015); higher temperatures are unnecessary and increase heat-illness risk.
There is little evidence supporting dehydration as a way of enhancing HA, or that HA improves performance in cool environments (Neal et al., 2016). It appears that HA is retained for at least 7 days (Neal et al., 2016) and any benefits that are lost within a month of HA are re-acquired with 2-4 further exposures (Weller et al., 2007).
Acute interventions
Hydration
Hypohydration impairs heat-loss, exacerbating negative effects of heat on performance. Therefore, individuals exercising in thermallystressful environments should aim to commence exercise in a
euhydrated state and prevent excessive dehydration (>2% bodyweight loss from water deficit). However, excessive drinking can cause hyponatremia, which is life-threatening and individuals should drink to thirst unless they have a prescribed fluid-strategy.
Pre- and per-cooling
Pre- or per- (during) exercise cooling techniques include: 1) external cooling, e.g. cool water immersion, cooling garments; 2) internal cooling, e.g. ingesting cold-liquids or ice-slurry; and 3) mixedmethods (multiple external and/or internal).
Pre-cooling strategies aim to reduce deep-body temperature by ~0.5-1.0 C, enabling greater heat-storage before hyperthermia develops. So long as a notable heat-sink is generated pre-cooling can be effective (Tyler et al., 2015). External cooling requires application of a cold medium to the skin sufficient to disrupt thermal equilibrium. Water immersion is often used, with temperatures of 12-18 C, durations of 20-30 minutes, and deep-body temperature monitoring for safety. However, decreased muscle and skin
temperature causes cutaneous vasoconstriction, diverts blood from active tissues and slows nerve conduction and muscle contraction, which can cause initial feelings of ‘sluggishness’. Vasoconstriction also causes diuresis, which is increased by hydrostatic pressure if water immersion is used. By ingesting cold-liquids or ice-slurry, internal cooling may reduce this ‘sluggishness’ and contribute
to hydration. Typically, 7.5 g kg-1 body mass of cold-liquids (carbohydrate/electrolytes) or ice-slurry are ingested in the 20-30 minutes before exercise. For a given volume, ice-slurry creates a larger heat-sink than cold-liquids because of the latent heat of fusion, but ingesting ice-slurry can be uncomfortable, reducing ad libitum drinking. Theoretically, mixed-methods should generate the greatest heat-sink, although this has received little attention. Few studies have employed a realistic ‘warm-up’; practitioners should consider the purpose and integration of warm-up within any precooling
intervention.
Although there is some evidence that per-cooling might inhibit normal thermoregulatory responses, this has not been demonstrated in a performance scenario. Indeed, per-cooling can be effective for enhancing exercise performance in the heat (Tyler et al., 2015). In some activities wearing cooling garments is possible during exercise. Phase change garments such as ‘ice vests’ may inhibit some evaporative heat-loss because skin contact is required for conductive heat-transfer and may be more appropriate when evaporative heat-loss is restricted, e.g. protective clothing. The effectiveness of ventilated vests is affected by the air ventilating the vest and is reduced with hotter and more humid air.
Perceptual manipulations
Some interventions induce sensations of coolness with minimal influence on thermal state. L-menthol, applied cutaneously, or swilled/ingested in drinks in low concentrations, stimulates cold receptors, although the evidence that this enhances performance is equivocal. Applying a cool medium to areas with high allesthesial thermo-sensitivity, e.g. ice-packs on the neck, can enhance performance with negligible cooling (Tyler et al., 2015). However, we advise caution with perceptual manipulations, which may result in dangerously high body temperatures whilst masking signs and symptoms of heat-illness.
Conclusion and recommendations
Performance in the heat can be improved by increasing or maintaining heat dissipation, reducing initial body-heat content or altering thermal perception. The optimal intervention(s) for an individual must be determined on a case-by-case basis taking into account the intervention mechanism, efficacy, practical and logistical constraints and safety issues (see Table 1). Any intervention should be practised before competition, under supervision of an experienced practitioner and with appropriate monitoring.
Dr Jo Corbett
Jo is an Associate Head and member of the Environmental and Occupational Research Group at the University of Portsmouth. He is a BASES accredited sport and exercise scientist.
Dr Oliver Gibson
Oliver is a Lecturer and member of the Centre for Human Performance Exercise and Rehabilitation at Brunel University London.
Dr Neil Maxwell
Neil is a Reader and leads the Environmental Extremes Laboratory at the University of Brighton.
Dr Caroline Sunderland
Caroline is a Reader and Director of the Sport, Health and Performance Enhancement Research Centre at Nottingham Trent University. She is a BASES accredited sport and exercise scientist.
Prof Neil Walsh
Neil is Director of the Extremes Research Group at Bangor University.
References:
Gibson, O.R. et al. (2015). Isothermic and fixed intensity heat acclimation methods induce similar heat adaptation following short and long-term timescales. Journal of Thermal Biology, 49, 55-65.
Neal, R.A. et al. (2016). Effect of permissive dehydration on induction and decay of heat acclimation, and temperate exercise performance. Frontiers in Physiology, 7, 564.
Mee, J.A. et al. (2015). A comparison of males and females’ temporal patterning to short- and long-term heat acclimation Scandinavian Journal of Medicine and Science in Sports, Suppl 1, 250-258
Tyler, C.J., Sunderland, C. & Cheung, S.S. (2015). The effect of cooling prior to and during exercise on exercise performance and capacity in the heat: a meta-analysis. British Journal of Sports Medicine, 49, 7-13.
Weller, A. et al. (2007). Quantification of the decay and re-induction of heat acclimation in dry-heat following 12 and 26 days without exposure to heat stress. European Journal of Applied Physiology, 102, 57-66.
Zurawlew, M.J. et al. (2016). Post-exercise hot water immersion induces heat acclimation and improves endurance exercise performance in the heat. Scandinavian Journal of Medicine and Science in Sports, 26, 745-754.
First published in The Sport and Exercise Scientist, Issue 53, Autumn 2017.
Published by the British Association of Sport and Exercise Sciences – www.bases.org.uk




Add comment